Diagnoses Treated
Addiction
The Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) recognizes two broad categories of disorders related to the use of psychoactive substances. Substance use disorders are syndromes of pathologic use of a substance; substance-induced disorders are disturbances of thinking, emotion, or behavior caused by intoxication with or withdrawal from a psychoactive substance.
Alcohol
Alcoholism affects approximately 10% of the population. Alcohol abuse or dependence usually develops during the first 5 years of regular use of alcohol. Three patterns of chronic alcohol abuse have been described as regular daily excessive drinking, regular heavy drinking on weekends only, and long periods of sobriety interspersed with binges that last days, weeks, or months. The major complication of alcoholism is suicide. More than 80% of individuals who kill themselves are depressed, alcoholic, or both. Alcohol is a frequent component of many suicides, even in patients who are not alcoholic. 75% of alcoholics have no other primary psychiatric diagnoses, although depression is a common complication of the direct effects of alcohol on the brain and the consequences of drinking on the patient’s life. Alcoholism may be an attempt at self-treatment of another psychiatric disorder, such as depression, anxiety, mania, psychosis, or post-traumatic stress disorder. This possibility should be considered when psychiatric symptoms clearly preceded heavy drinking. However, the history often is unreliable and only a trial period of abstinence reliably distinguishes between primary alcoholism and alcohol abuse that is secondary to another condition. If psychological distress resolves after a period of abstinence, alcoholism is likely to have been a cause rather than a result of the psychiatric disorder. Alcoholism is a common comorbid condition with mood disorders, anxiety disorders, and personality disorders. In such situations, both conditions must be treated.
Opioids
Opioid dependence and abuse is a major public health concern. The incidence of heroin use increased during the 1960s, and use of this drug is now a problem in smaller communities in the United States as well as in large cities. After a period of decreased use, narcotic use is undergoing a resurgence in middle class groups.
Anxiety Disorders
Anxiety is abnormal fear out of proportion to any external stimulus. Significant anxiety is experienced by 10%-15% of general medical outpatients and 10% of inpatients. Of the physically healthy population, 25% of individuals are anxious at some point in their lives. Approximately 7.5% of these people have a diagnosable anxiety disorder in any given month. Anxiety may be either a psychophysiologic response to a perception of internal or external danger or it may be spontaneous.
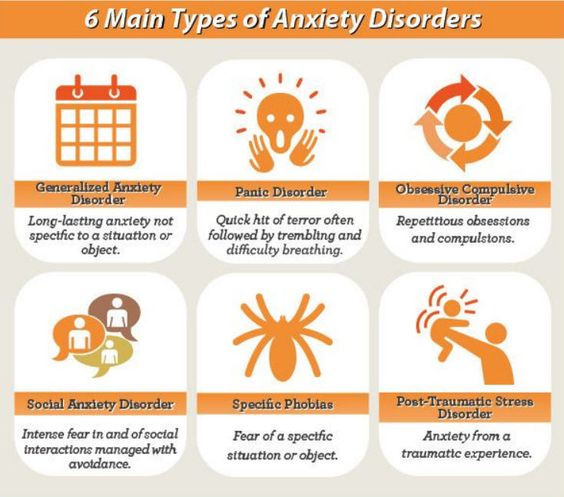

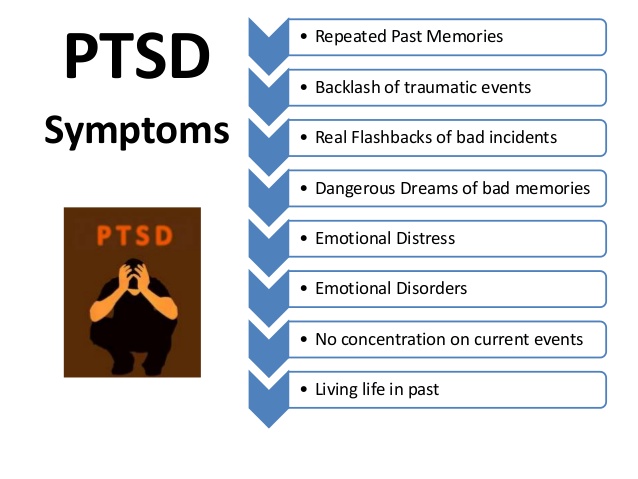
Post-Traumatic Stress Disorder (PTSD)
PTSD is a disorder that develops in some people who have experienced a shocking, scary, or dangerous event. Not every traumatized person develops ongoing (chronic) or even short-term (acute) PTSD. Not everyone with PTSD has been through a dangerous event. Some experiences, like the sudden, unexpected death of a loved one, can also cause PTSD. Symptoms usually begin early, within 3 months of the traumatic incident, but sometimes they begin years afterward. Symptoms must last more than a month and be severe enough to interfere with relationships or work to be considered PTSD. The course of the illness varies. Some people recover within 6 months, while others have symptoms that last much longer. In some people, the condition becomes chronic.
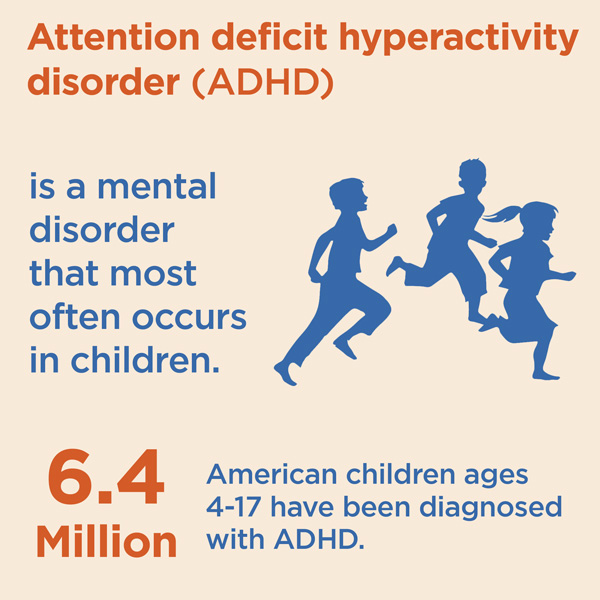
Attention Deficit Hyperactivity Disorder (ADHD)
Key symptoms of ADHD include a short attention span, difficulty concentrating, impulsivity, distractibility, excitability, and hyperactivity. Hyperactivity is defined subjectively as an increase in motor activity to a level that interferes with the child’s functioning at school, at home, or socially. It is important to note, however, that symptoms of attention deficit disorder may exist with or without hyperactivity.
Chronic Pain Syndromes
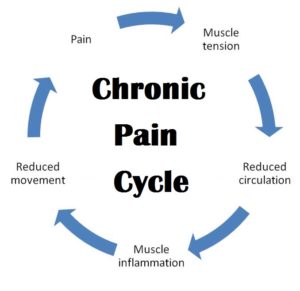
In most cases, chronic pain starts with an acute injury or illness. If the pain of this injury or illness lasts longer than six months, it’s then considered chronic pain. Sometimes, chronic pain subsequently causes complications. These complications, in turn, can make the pain worse. A chronic pain syndrome is the combination of chronic pain and the secondary complications that are making the original pain worse.
Chronic pain syndromes develop in a vicious cycle because of the cycle of pain causing pain; chronic pain that causes secondary complications, which subsequently make the original chronic pain worse. Chronic pain can lead to some common problems over time. For example, many people tend to have trouble sleeping because of pain. Chronic pain can also affect the roles people have in the family. They miss out on children’s activities, family functions, and parties with friends. As a result, many people struggle with guilt. Guilt isn’t the only emotion that is common to people living with chronic pain. Patients tend to report some combination of fear, irritability, anxiety, and depression. Patients also tend to express that they have lost their sense of direction to life.
These problems cause stress. These stressors can make the pain worse because stress affects the nervous system. It makes the nervous system more reactive and you become nervous. Pain is also a nerve related problem. Whatever the initial cause, pain travels along the nervous system to the brain, which is also part of the nervous system. Once reaching the brain, it registers as pain. When stress affects the nervous system, making it more reactive, the pain signals reach the brain in an amplified way, causing even more pain.
Complex Regional Pain Syndrome
Complex regional pain syndrome (CRPS) is a chronic (lasting greater than six months) pain condition that most often affects one limb (arm, leg, hand, or foot) usually after an injury. CRPS is believed to be caused by damage to, or malfunction of, the peripheral and central nervous systems. The central nervous system is composed of the brain and spinal cord; the peripheral nervous system involves nerve signaling from the brain and spinal cord to the rest of the body. CRPS is characterized by prolonged or excessive pain and changes in skin color, temperature, and/or swelling in the affected area.
The key symptom is prolonged severe pain that may be constant. It has been described as “burning,” “pins and needles” sensation, or as if someone were squeezing the affected limb. The pain may spread to the entire arm or leg, even though the injury might have only involved a finger or toe. In rare cases, pain can sometimes even travel to the opposite extremity. There is often increased sensitivity in the affected area, known as allodynia, in which normal contact with the skin is experienced as very painful.
People with CRPS also experience changes in skin temperature, skin color, or swelling of the affected limb. This is due to abnormal microcirculation caused by damage to the nerves controlling blood flow and temperature. As a result, an affected arm or leg may feel warmer or cooler compared to the opposite limb. The skin on the affected limb may change color, becoming blotchy, blue, purple, pale, or red.
Head Pain and Migraine Disorders
Headaches can be a chronic and recurrently incapacitating illness, symptoms of serious disease, or barometers of emotional stress. Their clinical importance lies also in their association with unusual symptoms, such as visual hallucinations, and in the contributing role, which is usually exaggerated, of psychologic factors. Almost three quarters of Americans have at least occasional headaches. Headaches together with backache and other benign pain disorders cause $55 billion in lost time every year.
Several varieties of chronic headache have distinctive patterns, are associated with unusual symptoms, and are affected by psychologic factors. These are muscle contraction (or tension) headaches, migraines, cluster headaches, postconcussive headaches, and trigeminal neuralgia (tic douloureux). Diagnosis in most cases is based not on physical or laboratory findings, which are usually normal, but on the patient’s description of the headache and of its response to particular medicines.

Insomnia
Insomnia can be caused by psychiatric and medical conditions, unhealthy sleep habits, specific substances, and/or certain biological factors. Recently, researchers have begun to think about insomnia as a problem of your brain being unable to stop being awake. Your brain has a sleep cycle and a wake cycle, when one is turned on the other is turned off. Insomnia can be a problem with either part of this cycle, too much wake drive or too little sleep drive. It’s important to first understand what could be causing your sleep difficulties.
There are many medical conditions (some mild and others more serious) that can lead to insomnia. In some cases, a medical condition itself causes insomnia, while in other cases, symptoms of the condition cause discomfort that can make it difficult for a person to sleep.
Sleep apnea is another sleep disorder linked to insomnia. With sleep apnea, a person’s airway becomes partially or completely obstructed during sleep, leading to pauses in breathing and a drop in oxygen levels. This causes a person to wake up briefly but repeatedly throughout the night. People with sleep apnea sometimes report experiencing insomnia. If you have trouble sleeping on a regular basis, it’s a good idea to review your health and think about whether any underlying medical issues or sleep disorders could be contributing to your sleep problems. In some cases, there are simple steps that can be taken to improve sleep; those steps include avoiding bright lighting while winding down and trying to limit possible distractions, such as TV, computer, or pets. While in either case, it’s important to talk to your doctor to figure out a course of action. You should not simply accept poor sleep as a way of life—talk to your doctor or a sleep specialist for help.
Insomnia can be caused by psychiatric conditions such as depression. Psychological struggles can make it hard to sleep, insomnia itself can bring on changes in mood, and shift in hormones and physiology can lead to both psychiatric issues and insomnia at the same time. Sleep problems may represent a symptom of depression, and the risk of severe insomnia is much higher in patients with major depressive disorders. Studies show that insomnia can also trigger or worsen depression. It’s important to know that symptoms of depression (such as low energy, loss of interest or motivation, feelings of sadness or hopelessness) and insomnia can be linked, and one can make the other worse. The good news is that both are treatable regardless of which came first.
Neuropsychiatric Lyme
Lyme disease is a multisystemic illness that can affect the central nervous system (CNS), causing neurologic and psychiatric symptoms. Up to 40% of patients with Lyme disease develop neurologic involvement of either the peripheral or central nervous system. Dissemination to the CNS can occur within the first few weeks after skin infection. Like syphilis, Lyme disease may have a latency period of months to years before symptoms of late infection emerge. Early signs include meningitis, encephalitis, cranial neuritis, and radiculoneuropathies. Later, encephalomyelitis and encephalopathy may occur. A broad range of psychiatric reactions have been associated with Lyme disease including paranoia, dementia, schizophrenia, bipolar disorder, panic attacks, major depression, anorexia nervosa, and obsessive-compulsive disorder. Depressive states among patients with late-Lyme disease are fairly common, ranging across studies from 26% to 66%. The microbiology of Borrelia burgdorferi sheds light on why Lyme disease can be relapsing and remitting and why it can be refractory to normal immune surveillance and standard antibiotic regimens.
Patients with late-stage Lyme may present with a variety of neurological and psychiatric problems, ranging from mild to severe. Lyme encephalopathy results in mood and cognitive disturbances as well as fatigue and a myriad of other symptoms such as headaches and sleep disorders. Cognitive difficulties include: simple and complex attention; slow visual and auditory processing; visual-spatial difficulties; sensory integration disorders; short-term and working memory difficulties; word-finding, word-generation and communication difficulties; decline in executive functions (planning and organization); confusion and decline in overall intellectual performance. Emotional/behavioral difficuties include: anxiety, panic attacks, depression, irritability, rage attacks, impulse dyscontrol, violent behavior, oppositional defiance disorder, sleep disorders, rapid mood swings that may mimic bipolarity (mania/depression), Obsessive Compulsive Disorder (OCD), Hyperactivity, Autism Spectrum-like disorders, antisocial disorders, and eating disorders.
Mood Disorders
Emotional symptoms of mood disorders are not the same for all people. Emotional symptoms of depression include thoughts of and attempts at suicide, loss of interest in activities that were pleasurable in the past, unyielding anxiety, sadness or feelings of emptiness, and feelings of worthlessness, helplessness, or guilt. Emotional symptoms of mania include prolonged periods of elation, restlessness, irritability, agitation, or excessive energy, feelings of grandiosity, and impulsive, risky, or hedonistic behavior.
As with emotional symptoms, physical symptoms of mood disorder may differ from one person to the next. Physical symptoms of depression include decreased energy or fatigue, headaches, body aches, pains, cramps or digestive problems, difficulty remembering details, difficulty making decisions and concentrating, loss of appetite or overeating, and excessive sleeping or insomnia. Physical symptoms of mania include racing thoughts and jumping from one idea to the next, pressured or rapid speech, increased goal-directed activities, insomnia, and hypersexuality.
Depression
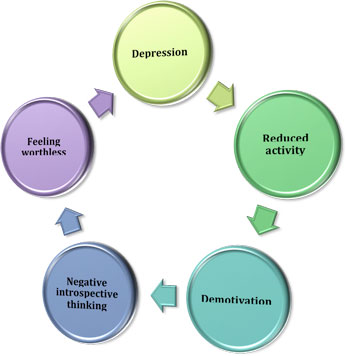
During severe depression, the systems that regulate emotion become disturbed. People in the middle of a severe depression often think only of things that are dark and sad. Physicians refer to this as “selective memory” – only remembering the bad times or the disappointments in life. This type of thinking is a symptom of the illness; it does not define who the person is. With proper treatment, the individual will start to remember the good times and develop a more positive outlook.
Suicidality
The most important thing to remember about suicidal thoughts is that they are symptoms of a treatable illness associated with fluctuations in the body and brain’s chemistry. They are not character flaws or signs of personal weakness, nor are they conditions that will just go away on their own. Depression and the depressive phase of bipolar disorder may cause symptoms such as intense sadness, hopelessness, lethargy, loss of appetite, disruption of sleep, decreased ability to perform usual tasks, and loss of interest in once-pleasurable activities.
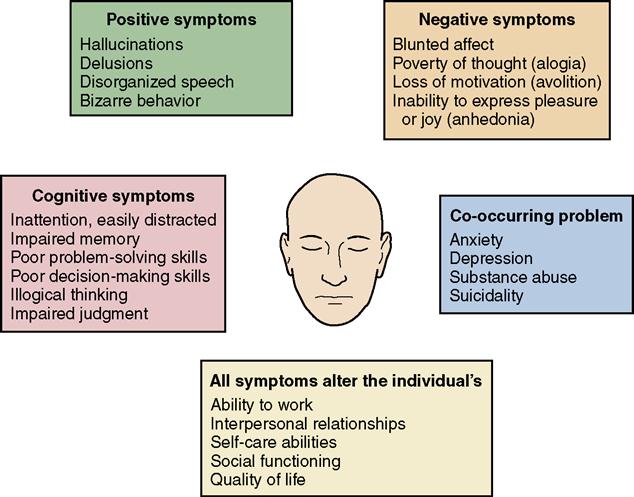
Thought Disorders
Schizophrenia is a disorder characterized by derangement of thought processes, affect, and behavior. The disorder involves expression of positive and negative symptoms. Positive symptoms are those that are added to the presentation such as delusions, hallucinations, catatonia, and agitation. Negative symptoms are those patient characteristics that appear missing from the presentation. This may involve affective flattening, apathy, social withdrawal, anhedonia, and poverty of thought and content of speech.